COPreDict

Development of COPD prognostic routine for optimal therapy prediction on the basis of lipid microbial biomarkers and AI-based modeling of immune response.
The COPreDict project aims at providing COPD patients and their doctors with a full-cycle support product, which includes a mobile application for patients that allows tracking their COPD progression status, and a clinical decision support system (CDSS) for doctors that allows personalized selection of prospective treatments for each patient case during exacerbation.
The mobile application will allow COPD patients to control their COPD status. In case of reaching critical health parameters, the App will immediately warn the patient about the necessity of visiting the doctor. In case of hospitalization and further exacerbation, the lipid-based microbial profile in the patient’s sputum and selected blood biomarkers will help to choose the best fitting therapy. The selected gene and protein biomarkers in the patient’s blood will be indicative of his/her immune status. Each combination of the microbial profiles and blood biomarkers will have its own corresponding treatment schema recommended for the respective patient cohort. The patient stratification guidelines and the associated treatment schemas will be a part of a specific AI-based Clinical Decision Support System developed within the COPreDict project.
Project coordinator:
Project partners:





Project overview
COPD facts
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable lung disease that is characterized by persistent airflow limitation and chronic respiratory symptoms. Major symptoms of COPD are dyspnea, chronic cough, and sputum production but extra- pulmonary manifestations such as fatigue and exercise limitation are also common. COPD is currently the third leading cause of death worldwide and is associated with high disease and economic burden. In 2016, the disease claimed 3 million lives worldwide, of which 300.000 deaths occurred in Europe. The direct healthcare costs of COPD are estimated to be €38.6 billion in Europe, excluding indirect costs such as COPD-related reduced workplace and home productivity. Continued exposure to risk factors as well as the ageing population are expected to contribute to an increased global COPD burden in the coming years.
COPD exacerbations
COPD exacerbations are part of the natural course of the disease and are defined as an acute worsening of respiratory symptoms that result in a need for additional therapy. Exacerbations are complex events and are usually associated with increased airway inflammation, mucus production, increased sputum volume and purulence, cough and wheeze, marked gas trapping, and hyperinflation. The heterogeneous aetiology of exacerbations has played a pivotal role in the identification of distinct biological exacerbation clusters. To date, four different clusters have been proposed: the infectious ‘bacteria-predominant’ and ‘virus-predominant’ clusters as well as the ‘eosinophil- predominant’ and ‘pauci-inflammatory’ clusters. Adequate recognition of exacerbations symptoms and early treatment is associated with faster recovery and better health-related quality of life.
COPD treatment strategies
Different maintenance pharmacotherapies exist to reduce symptoms, the frequency, and severity of exacerbations. Depending on the patient’s treatable traits, treatments differing in their mechanism (and duration) of action, route of delivery, inhaler types, or combination treatments may be prescribed. Common medications are bronchodilators (i.e. β2-agonists), anticholinergics (i.e. muscarinic antagonists), anti-inflammatory drugs (i.e. inhaled corticosteroids, oral glucocorticosteroids, and prophylactic antimicrobials), phosphodiesterase-4 inhibitors, and mucolytic agents. At present, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy document recommends treating mild exacerbations with short-acting bronchodilators, and moderate and severe exacerbations with antibiotics and/or oral corticosteroids.
The majority of exacerbations are currently not treated according to their aetiology but according to a one-fits-all approach. However, not all treatments may be necessary for all patients and for all exacerbations, and non-response to available treatments is common. Hence, despite the available pharmacotherapies a significant proportion of patients with COPD continues to experience exacerbations, which is associated with a high burden of disease. Only about 20–40% of all exacerbations have an eosinophilic inflammatory origin and respond well to systemic corticosteroids. With respect to the non-eosinophilic exacerbation clusters, those triggered by bacterial infections may require antibiotics. Currently, increased sputum volume and/ or purulence and dyspnea drive the decision for antibiotic treatment, although these assessments lack specificity. The guidance of antibiotic treatment is important since adverse effects such as antibiotic resistance and increased microbial dysbiosis should be avoided, particularly in frequent exacerbating patients who often receive antibiotics.
COPreDict project goals
The COPreDict project aims to develop a complex decision support system for doctors that will track the patient’s status of COPD progression via a number of clinically accepted COPD tests(such as COPD Assessment Test (CAT), Global Initiative for Obstructive Lung Disease (GOLD) Criteria for COPD, BODE Index for COPD Survival) integrated into a mobile app which will be daily used by the patient. These tests consider easy-to-measure parameters the patient can report to the app on a daily basis (such as heart rate after some physical exercises etc.) and the app will interpret the received info with an in-built calculator of COPD progression. Once negative dynamics will be observed in the patient’s measurements, the app will immediately inform the patient about a necessity to urgently see the doctor and all exacerbations in such case will be safely caught at a very early stage of development. This part of the COPreDict project will allow to detect the exacerbations on time and thus guarantee the start of early treatment.
Although most exacerbations have an infectious origin, the underlying mechanisms are heterogeneous and specific predictors of their occurrence in individual patients are currently unknown. Accurate prediction and early diagnosis of exacerbations is essential to develop novel targets for prevention and personalized treatments to reduce the impact of these events. Several potential biomarkers have previously been studied, these however lack specificity, accuracy and do not add value to the available clinical predictors. At present, microbial composition and host-microbiome interactions in the lung are increasingly recognized for their role in affecting the susceptibility to exacerbations, and may steer towards a novel direction in the management of COPD exacerbations. For this reason the COPreDict project brings its focus to identification of correlations between the bacterial profile of a given patient case using the sputum samples and the respective changes in the host transcriptome and cytokines profile from host’s blood samples. Identification of such correlations and stratification of COPD patients in respect to their bacterial profiles will allow to prescribe customized treatment schemas, predicted on the basis of integrated bacterial profiling and transcriptome analysis, and will significantly improve the current treatment schemas used, which are standardized for absolutely all patient cases without any difference.
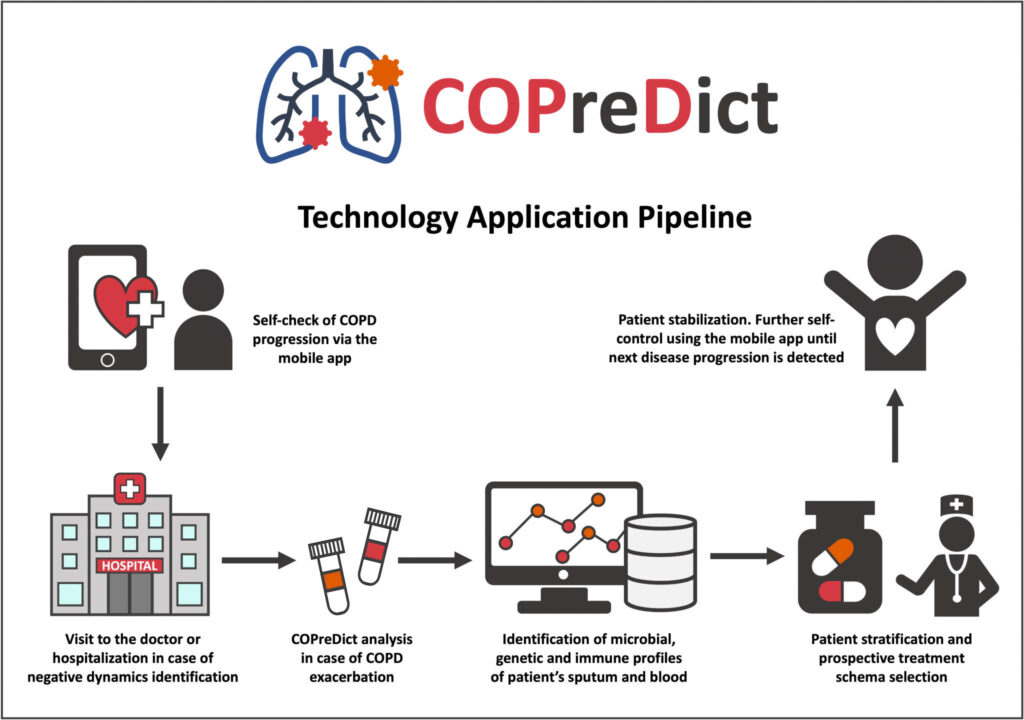
The project is aiming to develop a full cycle pipeline for the support of Chronic Obstructive Pulmonary Disease (COPD) patients allowing them to monitor their health status remotely via a phone App and further assist the medical doctors in selecting the prospective treatment for a particular clinical case if exacerbation of COPD has happened.
In the scope of the COPreDict project we will develop a decision support system for doctors that will allow to stratify the COPD patients into groups according to the microbiome profile identified in their sputum. The microbiome profile will be identified with the unique technique of measuring microbial lipid composition using the unique Mass Spectrometry of Microbial Markers (MSMM) method. MSMM as a reliable quantitative express method for diagnosing dysbacteriosis and identifying infectious agents which will be developed in this project for analysis of COPD samples. In addition to the bacterial profiling, the host gene profiling of the genes that will be identified as biomarkers of different COPD exacerbations subgroups will be carried out with the cheap RT-PCR method. The target genes will be identified on the basis of RNA-seq transcriptomics data analysis that will be performed on the publicly available data. In addition to bacterial profiling and gene expression profiling, the patient’s cytokines profile will be checked using the ELISA procedure. Integration of microbial profile, gene expression profile and cytokine profile will serve as the basis for patient stratification procedure, which will assign each of the patient groups with the respective prospective treatment schema.
Partners
Project partners:
ARCHI-MED GmbH
J.W. Goethe Universität Frankfurt
MOBILIST
ITTM
Coordinator
The project is coordinated by Dr. Alexander Kel, CSO geneXplain GmbH, Wolfenbüttel, Germany
Contract period
01.10.2022 – 30.09.2024
Contract no.
ZIM grant number KK5297004LU2
Further information
The project is aiming to develop a full cycle pipeline for the support of Chronic Obstructive Pulmonary Disease (COPD) patients allowing them to monitor their health status remotely via a phone App and further assist the medical doctors in selecting the prospective treatment for a particular clinical case if exacerbation of COPD has happened.
In the scope of the COPreDict project we will develop a decision support system for doctors that will allow to stratify the COPD patients into groups according to the microbiome profile identified in their sputum. The microbiome profile will be identified with the unique technique of measuring microbial lipid composition using the unique Mass Spectrometry of Microbial Markers (MSMM) method. MSMM as a reliable quantitative express method for diagnosing dysbacteriosis and identifying infectious agents which will be developed in this project for analysis of COPD samples. In addition to the bacterial profiling, the host gene profiling of the genes that will be identified as biomarkers of different COPD exacerbations subgroups will be carried out with the cheap RT-PCR method. The target genes will be identified on the basis of RNA-seq transcriptomics data analysis that will be performed on the publicly available data. In addition to bacterial profiling and gene expression profiling, the patient’s cytokines profile will be checked using the ELISA procedure. Integration of microbial profile, gene expression profile and cytokine profile will serve as the basis for patient stratification procedure, which will assign each of the patient groups with the respective prospective treatment schema.


